Kev
Whoever feeds you controls you.
Parasitic zoonoses are diseases caused by parasitic organisms that can be transmitted from animals to humans. Parasites such as protozoa, helminths, and arthropods can cause a range of illnesses in humans, from mild discomfort to severe disease. The most common parasitic zoonoses are toxoplasmosis, malaria, leishmaniasis, giardiasis, and cryptosporidiosis.
These diseases are usually transmitted to humans through contact with contaminated animal feces, contaminated food or water, or through the bites of infected insects and other vectors. In addition, people who work with animals, such as farmers, veterinarians, and animal handlers, are at increased risk of contracting parasitic zoonoses.
In this post, we are going to take a loook at a few parasitic zoonoses of importance in food.
Adult parasite (tapeworm) causes taeniasis while the larval stage causes cysticercosis. The adult stage is usually hosted by humans while the larval stage is found in animals (especially the domesticated ones).
The intermediate host is domestic animals like cattle and shoats (sheep and goats).
There are two prominent species of the tapeworm:
People can harbour both the larval and adult stages of Taenia solium. Humans are the immediate and permanent host of the worm. Human to human transmission does not occur.
Taenia solium eggs are transferred to other hosts through food.
Life cycle of Taenia spp. worm

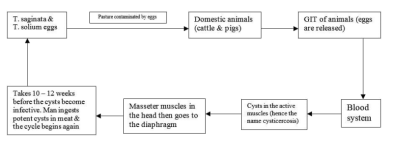
The life cycle of these two worms can begin anywhere within the cycle.
In animals, conduct post-mortem tests and evaluate the cyst count. If the cyst count is less than 10, the meat is not condemned but sold under instruction. If the cyst count is greater than 20, condemn the meat.
People should undergo regular deworming to eradicate the worm.
Echnococcosis is caused by two strains of echnococcus that inhabit dogs. The two strains are:
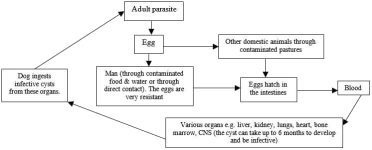
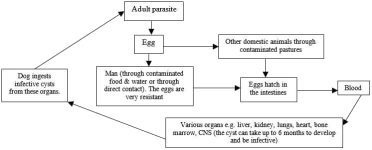
Life cycle of the hydatid parasite

The causative protozoan is Toxoplasma gondii.
The cat being the definitive host of the microorganism sheds the oocytes through the faeces. The oocytes sporulate once they come into contact with air.
Humans get the infection through the spores since they have a close association with cats. They can get into contact with the spores through:
In humans, perform serological tests.
Horses also get the disease. Dogs, cats, and other carnivores also get the disease but they may not transmit it to humans.
People get the cyst from boar/bear/horse meat. When the cyst gets into the stomach, it vegetates and grows into an adult. It then passes into the intestines where it lays eggs.
Immature larvae will get into the blood and then pass into the muscles.
Break the cycle of the nematode to discontinue infection cycle.
These diseases are usually transmitted to humans through contact with contaminated animal feces, contaminated food or water, or through the bites of infected insects and other vectors. In addition, people who work with animals, such as farmers, veterinarians, and animal handlers, are at increased risk of contracting parasitic zoonoses.
In this post, we are going to take a loook at a few parasitic zoonoses of importance in food.
1. Taeniasis / Cysticercosis
Parasitic zoonoses are associated with meat. Psychrozoonoses require more than one vertebrate host to cause a disease.Adult parasite (tapeworm) causes taeniasis while the larval stage causes cysticercosis. The adult stage is usually hosted by humans while the larval stage is found in animals (especially the domesticated ones).
The intermediate host is domestic animals like cattle and shoats (sheep and goats).
There are two prominent species of the tapeworm:
- Taenia solium
- Taenia saginata
- saginatamajorly inhabits cattle but can also be found in other animals.
People can harbour both the larval and adult stages of Taenia solium. Humans are the immediate and permanent host of the worm. Human to human transmission does not occur.
Taenia solium eggs are transferred to other hosts through food.
Life cycle of Taenia spp. worm

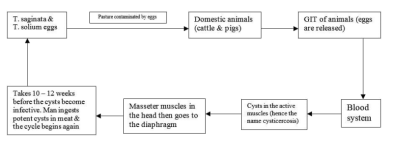
The life cycle of these two worms can begin anywhere within the cycle.
Clinical signs and symptoms of taeniasis
- Taeniasis in an adult human being is asymptomatic except for pains and weight loss. High infection in children will cause other symptoms. Ulcer pains due to hooks in the intestines that cause bleeding.
- Diarrhoea with dysentery
- Nausea and vomiting in adults
- Psychological disturbance (adults do not want to admit that they have worms).
- The larval stage of Taenia solium will produce serious signs, especially when it gets into the brain.
- Some of the observable symptoms include:
- Severe headache
- Nausea and vomiting
- Blurred vision that may lead to blindness
- Feeling of numbness
- Cystircercosis in animals will be manifested as cysts in the masseter muscles and cardiac muscles.
- The disease in animals may be sub-clinical, only to be noted during post-mortem.
Diagnosis of taeniasis
Analyse the stool for the eggs in humans.In animals, conduct post-mortem tests and evaluate the cyst count. If the cyst count is less than 10, the meat is not condemned but sold under instruction. If the cyst count is greater than 20, condemn the meat.
Treatment of taeniasis
In animals, the disease is not treated as they do not show clinical signs.People should undergo regular deworming to eradicate the worm.
Control measures for taeniasis
- Inspect meat before consumption.
- Proper disposal of human waste
- Cook meat properly before consumption
- Regular deworming of people (3 months interval).
2. Hydatidosis / Echnococcosis
Hydatidosis is caused by hydatid cyst. The larval stage affects both humans and animals.Echnococcosis is caused by two strains of echnococcus that inhabit dogs. The two strains are:
- Echnococcus granulosus
- Echnococcus multicularis
Life cycle of the hydatid parasite

Symptoms of hydatidosis in dogs
- Severe enteritis under severe infestation
- Diarrhoea with blood
- Anaemia in young puppies
- Rough hair coat
Clinical signs of hydatidosis in humans
- The cysts cause organ enlargement leading to an enlarged abdomen
- Organ failure may occur depending on the level of infestation
- When the severity reaches the CNS, nervous symptoms occur.
Diagnosis of hydatidosis
- Use faecal sample for analysis.
- It is not possible to diagnose domestic animals. The cysts will be seen in the organs when the animals die.
- In humans, suspect the disease from the symptoms, especially abdominal enlargement.
- Confirmation of infection by scanning the organs for cysts. Serological tests are also applicable.
Treatment of hydatidosis
- Deworm dogs using an anthelmintic
- Domestic animals do not show symptoms hence no treatment
- In humans, surgical procedures are applicable. The procedure should be very delicate because the worms contain a very toxic fluid.
Control measures for hydatidosis
- Proper meat inspection
- Regular deworming of dogs
- Minimize contact between humans and dogs
Summary table for the three worms
| Adult host | Definitive host | Organs affected | Larval stage | Intermediate host | Organs affected |
| T. saginata | Man | Intestines | C. bovis | Shoats & cattle | Active muscles (e.g. tongue, diaphragm |
| T. solium | Man | Intestines | C. cellulosae | Pigs | Muscles |
| Echnococcus | Dog | Intestines | Hydatid cyst | Humans & domestic animals | Soft organs like liver |
Toxoplasmosis
This is a protozoan disease that affect all domestic animals. The infection is critical when the infection enters the cat because the cat hosts the infective stage of the disease.The causative protozoan is Toxoplasma gondii.
The cat being the definitive host of the microorganism sheds the oocytes through the faeces. The oocytes sporulate once they come into contact with air.
Humans get the infection through the spores since they have a close association with cats. They can get into contact with the spores through:
- Consumption of contaminated foods
- Inhaling the spores in the air
- Congenital transmission (mother to child through the placenta)
Clinical signs of toxoplasmosis in animals
- Animals exhibit the inapparent form of the disease.
- Epidemics occur in rare cases when the disease occur in chickens, pigs, and rabbits
- In shoats (sheep and goats), the disease trigger abortions
Clinical signs of toxoplasmosis in humans
Symptoms usually vary with age.- Adults get inapparent form of the disease
- Pregnancy in women activates the disease and the patient has pneumonia and swollen lymph nodes. The CNS may be affected and the pregnancy may end up in an abortion or a stillbirth.
- Babies born of infected mothers’ exhibit generalized infections immediately after birth. They developed enlarged liver and spleen and may experience convulsions. Babies who survive may be mentally retarded.
- Young children who acquire the infection from a cat may experience general malaise and mild infections.
Diagnosis of toxoplasmosis
In animals, examine the faecal sample for the oocytes.In humans, perform serological tests.
Control measures for toxoplasmosis
- Pregnant women should ensure strict and paramount hygiene when handling cats
- Young children should avoid close contact with cats
- People should avoid raw and under-cooked meat
- Avoid feeding cats with raw meat
- Control vectors such as flies and cockroaches.
Trichinellosis
Trichinellosis is a parasitic zoonotic disease that is directly transmitted from animals to humans. The causative organism is a nematode called Trichinella spiralis.Epidemiology of trichinellosis
The disease majorly occurs in the northern hemisphere. It is very prevalent in Alaska and places where people love wild boar and bear meat.Horses also get the disease. Dogs, cats, and other carnivores also get the disease but they may not transmit it to humans.
Life cycle of the Trichinella spp. nematode
The disease undergoes a similar cycle in humans as in animals.People get the cyst from boar/bear/horse meat. When the cyst gets into the stomach, it vegetates and grows into an adult. It then passes into the intestines where it lays eggs.
Immature larvae will get into the blood and then pass into the muscles.
Sources of trichinella infection
This disease is majorly transmitted through garbage and feeding. Some of the most common routes of transmission include:- Consumption of raw / improperly cooked meat (from boar/bear/horse)
- People who feed garbage to pigs perpetrate the disease
- Birds eat garbage and spread the disease through their eggs and droppings
- Domestic animals may also get and transmit the disease when they scavenge through garbage.
Symptoms of trichinellosis in humans
When the nematode is still in larval stage, the patient may experience the following:- Nausea
- Abdominal discomfort
- Fever
- Headaches
- Facial oedema
- Itchy skin
- Myositis in the muscles (irritation and pain of the muscles)
- Pain and irritation of the tongue, masseter muscles, diaphragm, and the heart muscles
- If the disease reaches the lungs, the patient will experience dyspnoea and coughing.
- The patient may feel tired due to improper circulation when the disease affects the heart.
Symptoms of trichinellosis in animals
The adult parasite resides in the stomach. The sick animal will show the following signs:- Abdominal discomfort
- Diarrhoea
- General sickness
- Myositis in the muscles depending on the affected muscles
- Difficulty in breathing if the disease affects the diaphragm
- When the disease affects the masseter muscles, the animal will have difficulty in feeding
- The animal will tire if the heart is affected
Diagnosis of trichinellosis
Examine the faecal sample for the eggs of the parasite.Treatment of trichinellosis
Regularly deworm the animals and peopleBreak the cycle of the nematode to discontinue infection cycle.
Control measures for trichinellosis
- Regular testing and treatment of sick patients. Treat any animal in whose faecal sample you find one egg
- Proper garbage disposal and management
- Avoid feeding pigs on garbage
- Proper cooking of meat
- Deep freezing can help eliminate the parasite.
Last edited:
