Understanding Food-borne Illnesses
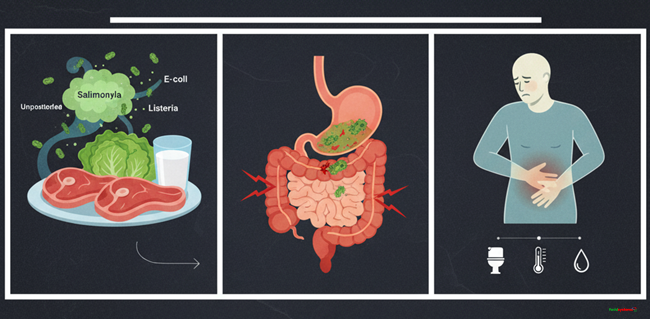
According to World Health Organization, food borne diseases are those diseases that enter the host through food; especially those that affect man and cause poisoning in animals.
They are of two types, namely:
- Food-borne infections and
- Food-borne intoxications
Food-borne Infections and Intoxications
Food-borne infections occur through consumption of contaminated foods or beverages. On the other hand, food intoxication occurs when toxic chemical substances of microorganisms in food get into man’s system.
While some like mushroom, fish, and cassava may be primarily toxic, others like molluscs have secondary toxicity. When an animal eats a mollusc, it produces chemical substances that cause toxicity to their secondary host.
Food additives may also become poisonous in food during production.
Sources of food contamination
There are many sources of food contamination and various stages of the food chain including production, transport, processing, storage, and consumption levels.
The most common sources include:
i) Food animals (edible)
These may contain infectious organisms in their intestines and/or muscles that cause food contamination.
ii) Meat
May be contaminated during slaughtering or handling.
iii) Fresh fruits and vegetables
When grown in contaminated soils, these can be a source of food contamination. Contamination can also set in during handling when contaminated water is used to clean the produce.
iv) Eggs
When the hens feed on heavy metals or feed that is contaminated with chemicals, the contaminant is transferred to the final consumer through the eggs.
v) Seafood
Seafood is notorious for heavy metal contamination.
vi) Infected humans
May introduce the contamination during handling of food. The most notorious case is tuberculosis.
vii) Cross contamination
Happens when one contaminated food is mixed with a different clean food. Happens mostly during handling of raw food or during cooking.
Foods that are commonly associated with food borne diseases
- Food animals; especially those that people tend to consume in their raw state like meat, fish, or milk.
- Foods that mix animal products e.g. milk, eggs, and minced meat.
- Fruits and vegetables since people tend to consume most of them raw.
- Fresh manure when used in a vegetable farm to increase soil fertility may contaminate the plants.
People who are at risk of food-borne infections include:
It is important to note that food-borne diseases pose a risk to every living soul. However, there are those individuals with increased risk to infection than others.
For instance, people who handle animal products are at a higher risk due to their increased levels of exposure.
Pregnant women, the elderly, infants, and people with compromised immunity are at a higher risk as well.
General symptoms of food-borne disease infection and general prevention measures
Most of these infections take the oral route because they tend to be consumed with the food. When infected, you will notice any or a combination of the following:
- Nausea
- Vomiting
- Abdominal pain/cramps
- Diarrhoea
To reduce the risk of infection, you can ensure the following:
- Sufficient cooking of all foods, especially for animal products.
- Proper preservation – refrigerate or freeze all foods of animal origin
- Keep foods in separate containers (avoid mixing foods)
- Use clean and sterile equipment and work surface when handling food. This goes for the water used as well.
It is usually not easy to trace the origin of an outbreak because it is not easy to tell where you might have picked an infection.
Food-borne infections could be caused by strict human pathogens such as Salmonella typhimurium or pathogens that affect both man and animal such as Salmonellosis. Either way, it is important to be safe.
Some of the very common food borne diseases and infections include:
1. Salmonellosis
This is a bacterial infection that affects both man and animal.
Aetiology (cause)
Salmonella bacteria have very many strains (over 1700) with potential to harm man and animal. It is gram negative, rod-shaped, non-lactose fermenter enterobacteria.
Salmonella typhimurium is the most common strain that affects man while Salmonella dublin causes disease in animals.
Sources
The primary source is in the intestines and they are shed in faeces. Animals and man can harbour this disease without showing any signs hence they become chronic carriers.
In such cases, the organisms reside in the gall bladder, liver, and spleen. The diseases causing microorganisms in these animals are usually transferred during slaughter.
Where commonly found
- Meat and meat products such as beef, mutton, etc.
- Pork (between 2 – 5 percent of all slaughtered pork contains Salmonella typhimurium in their lymph node hence continues to contaminate the rest of the products during processing).
- Poultry has the highest contamination by Salmonella typhimurium in their intestines,
- Eggs and egg products (especially duck eggs) pose a great danger when cracked.
- Milk and milk products contain both typhimurium and S. dublin especially during warm weather and in farms that use poor milking techniques.
- Direct contact with animals, animal products and carcasses of infected animals.
- Water contamination from faeces
- Pests and rodents who are the intermediaries for the disease especially when they come into contact with animals and food.
Clinical signs in animals
The condition is more prominent in young stock than adults that can harbour it without showing any symptoms. The symptoms include:
- Anorexia
- Dullness
- Slight fever
- Severe diarrhoea (initially watery then dysentery sets in)
- Dehydration (the animals become so weak, their skin wrinkles and death follows.
Symptoms in man
In man, the disease incubates for about 36 -72 hours before showing any signs. The symptoms include:
- Abdominal pains
- Diarrhoea with chills
- Vomiting
- Fever
- Headache
- Prostration (weakness)
- Septicaemia, which may lead to cardiac failure
Note: the severity of the symptoms depends on the dosage of the microorganism and the age of the patient.
Diagnosis and treatment
Diagnosis is done at a medical facility through lab testing. The doctor prescribes treatment depending on the lab results.
Control measures
- Properly cook animal products
- Ensure hygienic handling of all animal products
- Use proper milking and milk handling techniques.
- Never wash eggs when they are cracked
2. Typhoid Fever and Paratyphoid
Caused by two strains of Salmonella bacteria that are strictly human pathogens. They are;
- S. typhi (typhoid fever) and
- S. paratyphi (paratyphoid).
Aetiology
The pathogens are strictly human pathogens, especially for those who carry the disease.
The disease reaches the chronic carrier state where the hosts retain the bacteria in the gall bladder and GIT.
It affects middle-aged women more than any other group of human beings.
Transmission
- Contaminated water and foods e.g. milk, fruits, and vegetable.
- Can be shed through stool and urine
- Mechanical transfer by insects from one food to the next
Symptoms
Incubation period for typhoid fever is between 3 – 28 days while paratyphoid incubates for between 1 -15 days. The observable symptoms include:
- Septicemia
- Slight fever (up to two weeks). After the 2 weeks, the organism moves from the blood into the GIT affecting the lymph nodes leading to severe abdominal pains.
- Nausea
- Vomiting
- Diarrhoea
- Rosebuds (petcheatons)
- Breaking of capillaries
- Kidney failure
Fatality rates in humans average 10 percent annually.
Diagnosis
Suspect the disease from the symptoms. Isolation of the bacteria from the stool is a confirmatory test for the disease. The organism can also be isolated from the blood by culturing.
Serological tests (checking the actions of antigens against this organism) can also confirm the disease.
Treatment
Seek medical attention in a hospital. Good nursing care is important for quick healing.
Control measures
- Proper sewage disposal
- Use boiled water for domestic consumption
- Wash fruits and vegetables with clean boiled water
- Consume only properly pasteurized milk
- Test and treat chronic carriers
- Vaccinate people (vaccines will give 2 – 3 years of protection)
Where there is a massive outbreak of this disease, people will still get it.
3. Shigellosis
It is also referred to as Bacillary Diarrhoea and is caused by a strict human pathogen.
This disease breaks out depending on geographical locations. You may not get it depending on where you stay.
It occurs in temperate countries (where it also slowly disappearing).
Aetiology
About four sub-species of the Shigellae spp are culprits. However, Enterobacteriaceae spp is the most pronounced. It produces potent toxin that affects the host.
Sources
Humans are the most common carriers. However, monkeys have been reported to carry the organism in some areas.
It occurs mainly in children, young adults and the elderly.
Foods commonly associated with this infection include:
- Milk and milk products
- Raw vegetables
- Fish
When the infection occurs, it is common to pass it from one person to the next in 80 percent of the cases. This is not very common with food infections.
Symptoms
The organism requires a very small dose to cause a disease. The bacteria attach itself to the walls of the intestines where they multiply and produce toxins.
The toxins cause toxaemia, which spreads to other parts of the body.
Some of the common symptoms include:
- Diarrhoea that comes on and off
- Mild abdominal pains; you may pass a few loose stools
- Nausea for people with HIV
- Watery stool with mucus/pus and stained with blood.
- An agonizing pain (colic) and temptation to diarrhoea (tenesmus)
- Fatality is low but the rate increases in children, the elderly, and people with compromised immunity.
- Patients take long to recover (about 3 months).
Diagnosis
Check the bacteria in the stool and isolate it.
Treatment
Seek medical help from a medical facility and use antibiotics. Fluid replacement (hydrotherapy) is critical.
Control measures
- Maintain high standards of personal hygiene
- Boil water before using it for consumption purposes
- Proper sewage treatment and disposal is key
- Properly pasteurize milk before consumption
- Proper handling and cooking of vegetables
4. Haemorrhagic Colitis
This food borne disease is an enteropathogenic Escherichia coli infection that affects both man and animals. It is widespread in man and is very common in infants under poor sanitary conditions.
The specific strain that causes disease is E. coli 0157H.
When the bacteria cause disease in animals, the condition is referred to as colibacillosis.
Colibacillocis will occur in small animals between 1 – 14 days. They get a very serious disease that is commonly referred to as Septicaemic coli. The bacteria use the navel as the route of infection.
The disease may also affect the nervous system. It usually has very high fatality rates.
Animals that manage to recover harbour the organism in the joints leading to arthritis. If the bacteria hide in the brain, they cause meningitis, while those that hide in the lungs will cause pneumonia.
Ophthalmitis occurs if the bacteria harbours in the eyes of animals that manage to recover and enteric colibacillosis is the disease that affects animals aged between 3 – 8 months.
Predisposing factors
- Overcrowding
- Poor housing
- Poorly lit and ventilated room
- Poor waste management (including animal droppings and sewage)
- Poor feeding management
- Overfeeding young calves with colostrum gives the physiological diarrhoea, which impairs their immunity.
- Poor hygiene management and poor milking techniques.
Sources
Intestines of animals and will be shed through faeces that contaminate water and soil. Pathogenic strains are very resistant and remain potent for long.
If any food product comes into contact with contaminated water, soil or faeces, it becomes a source of contamination.
In institutions where kids are fed using feeding bottles, there is a risk of spreading the disease if only one bottle is contaminated.
Symptoms
Incubation period is 2 – 4 days.
The bacteria attack the epithelial cells and produce toxin that causes gastroenteritis. The observable symptoms include:
- Sudden onset of severe stomach pains with cramps followed by watery blood-stained diarrhoea.
- Vomiting
- Small fever
- Fatality is not very common
- The disease may progress for a week if not treated. In which case, other strains of E. coli will cause other illnesses including:
Travellers’ diarrhoea, which is usually associated with consuming unhygienic foods while travelling.
Haemolytic uremic syndrome, which is an equivalent of Septicaemic coli.
It has high fatality rates of up to 50 percent. People that manage to recover may suffer from kidney failure if the organism is logged in the kidney. Those that manage to recover may be forced to undergo dialysis for the rest of their lives.
Diagnosis
Culture the stool. It should have a high plate count.
Treatment
Hospitalization for early treatment.
Rehydration to replace the lost electrolytes and restore normal balance.
Adults may pass to notice the symptoms of the disease.
Control measures
- Maintain strict hygiene
- Encourage breastfeeding and maintain high standards of hygiene for the feeding utensils.
- Properly cook meat and meat products, milk, and eggs. Wash vegetables and fruits properly before consuming them.
- Use boiled water for domestic activities.
5. Cholera
Of all the food borne diseases, cholera is one of the most ravaging. It is caused by a strict human pathogen that spreads fast and affects many people. It usually leads to epidemics with mortality rates of up to 30 percent.
Aetiology
Caused by Vibrio cholera. The typical biotype E1 and TOR.
Epidemiology/Sources
Spread through contaminated water and the bacteria survives longer in an alkaline condition. Acidic conditions usually kill it.
It is common for this disease to occur in crowded areas. It is usually associated with symptomless carriers.
Pathogenicity is very clear. The organism is ingested through water. Once it reaches the intestines, it multiplies fast and produces an enterotoxin that causes severe enteritis (inflammation).
Symptoms
One requires a very small dose for the disease to occur. Incubation takes between 3 – 12 hours. The observable symptoms include:
- Sudden onset of effortless vomiting followed by profuse diarrhoea (between 20 -30 times in a day), which leads to rapid dehydration.
- “Rice” watery diarrhoea when small bits of mucosa is present in the stool
- Severe dehydration that leads to suppression of urination. The patient develops wrinkled skin, sunken eye sockets and becomes very weak.
- Lowering of the blood pressure leading to rapid and weak pulse. This may lead to circulatory failure and death.
Diagnosis
- The bacteria are very easy to identify because it is filamentous and motile.
- Cultural isolation of the stool or water can be effective as well.
- Serological testing (titrating the antigen/antibody reaction) can be used to identify the microorganism.
Treatment
Immediate hospitalization. Medication with antibiotics and rehydration is very critical to survival of the patient.
Control measures
- Maintain personal hygiene
- Boil/treat the water you intend to use for domestic consumption
- Proper sewage disposal
- Hygienic handling of foods
- Vaccination (effective for six months).
Atypical Cholera
Caused by Vibrio parahaemolyticus. It is usually associated with marine life and sea foods are the major culprits of the microorganism.
It incubates for 12 hours
Symptoms
- Abdominal pain
- Nausea
- Vomiting
- Diarrhoea
The disease is not as severe as typical cholera and it can end without medical intervention.
Control measures
- Avoid consumption of poorly prepared sea food
- Freeze the sea food; it kills these microorganisms
- Avoid mixing raw with cooked food.
Food-Borne Viral Infections
1. Infectious Hepatitis
Hepatitis is a common / prevalent infection that is easy to diagnose. It is caused by virus types A and B.
Aetiology
When the disease occurs, the virus is shed through the blood, stool, and urine of the infected person.
The disease is more severe in children. Adults experience a protracted period of the disease.
Transmission
Majorly transmitted through oral consumption of contaminated water by stool or urine of an infected person.
You can also get it through contact with the blood of an infected person.
Hepatitis type B can be transmitted through sexual contact.
Symptoms
Incubation period is between two and six weeks.
It takes quite long to get a slight manifestation. Some of the noticeable symptoms include:
- Slight increase in body fever
- General malaise
- Faintness and weakness
- Anorexia
- Nausea
- Abdominal discomfort
- Liver failure symptoms (jaundice)
- Ascites (accumulation of fluid in the abdomen)
- Changes in urine colour due to presence of bile
Diagnosis
Once the incubation period is complete, the onset of the symptoms is characteristic.
Test the liver functions and identify the virus in the blood or urine through cultural isolation.
Control measures
- Vaccination is the most effective way.
- Maintain high hygiene standards for food, water, and self.
- Proper sewage treatment and disposal channels.
2. Poliomyelitis
This disease can occur in apparent forms (i.e. cases where the disease is present but the patients do not show any symptom). It is caused by polio virus 1, 2, and 3.
Aetiology
The virus is shed through the stool and pharyngeal excretions. People catch the virus through consumption of contaminated water, milk, and other fluid foods.
Symptoms
Incubation takes between seven and 10 days.
- It starts with fever followed by headache
- General malaise
- Constipation
- Stiffness of the neck
- Paralysis of limbs
- Meningitis may also occur
Diagnosis
The symptoms are helpful in making a tentative diagnosis.
Isolate the virus from the stool and other secretions of the body.
Serological tests are also helpful in diagnosing this disease.
Control measures
- Vaccination is very effective; done only once and remains effective for life.
- Maintaining high standards of personal hygiene is crucial. Food and must be kept clean and uncontaminated.
General Disease Control Methods
i) Increasing the host resistance
You can achieve this in two ways:
- Proper and improved nutrition
- Vaccination
ii) Taming the environment
Here, you eliminate or reduce the hazards / predisposing factors to the disease. You can achieve this through environmental sanitation, e.g.
- Water should be safe and adequate
- The housing should be sound to eliminate physical and biological hazards
- Food hygiene should be high throughout all the stages of production. Check and control the type of soil, the food storage premises, and even the chemicals used in production. Inspect and reduce all sources of contamination (including the health of human handlers). Refrigerate stored foods at the right temperature.
- Conduct mass education on food hygiene
- Disinfect areas where the sick animals stay to avoid contamination and cross-contamination to a healthy host. You can use chemical disinfectants or irradiation for this purpose.
- Practice proper waste and sewage disposal. Properly manage and dispose industrial wastes as well
- Control the quality of the air you breathe through sanitation or filtering
- Minimize contact with animals to reduce chances of spread of zoonotic diseases






Responses